OVERVIEW
Healthcare is increasingly shifting towards ease of access and patient empowerment. Simultaneously, emerging health threats are intercalating into our daily lives, forcing a reimagining of pandemic preparedness. To remain agile in our response to new threats, we need to build upon what is succeeding today. The future is now, mandated and accelerated by COVID-19, where novel health ecosystems and can be leveraged, vast amounts of health data can be accessed, and successes of health product investments can be measured not just by regulatory approval but by the clinical impact they have every day.
CURRENT PROJECTS
Decentralized Clinical Studies and Healthcare Delivery Models
The HI-3 program is interested exploring the utility of decentralized care models. The COVID-19 pandemic has accelerated new opportunities for patients to access health care in more convenient settings like retail clinics or at home via telehealth. Simultaneously, it highlighted the difficulties of implementing clinical studies, especially for products designed for use in settings outside of the hospital. Decentralized healthcare models have the potential to vastly improve both patient recruitment for clinical studies during public health emergencies and improve patient access to care. DRIVe is interested in leveraging such an ecosystem for:
- 1) Validating technologies in real world environments
- 2) Leveraging commercial health data for new insights
- 3) Testing new healthcare delivery models
For more information on this opportunity, please view our D-COHRe Strategic Partnership page.

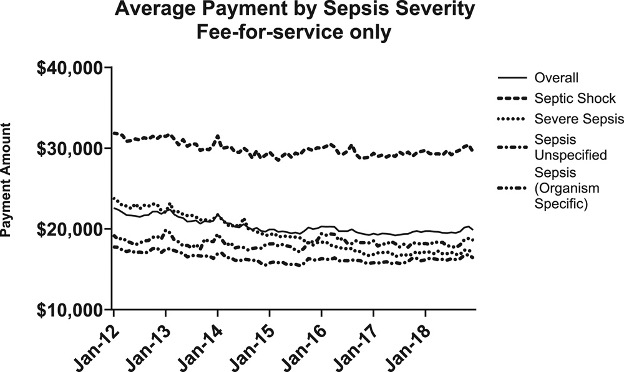
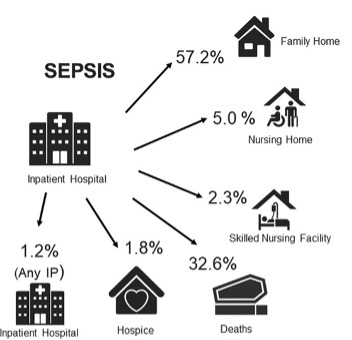
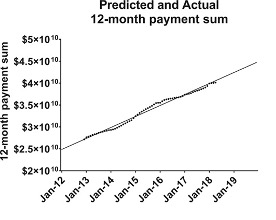
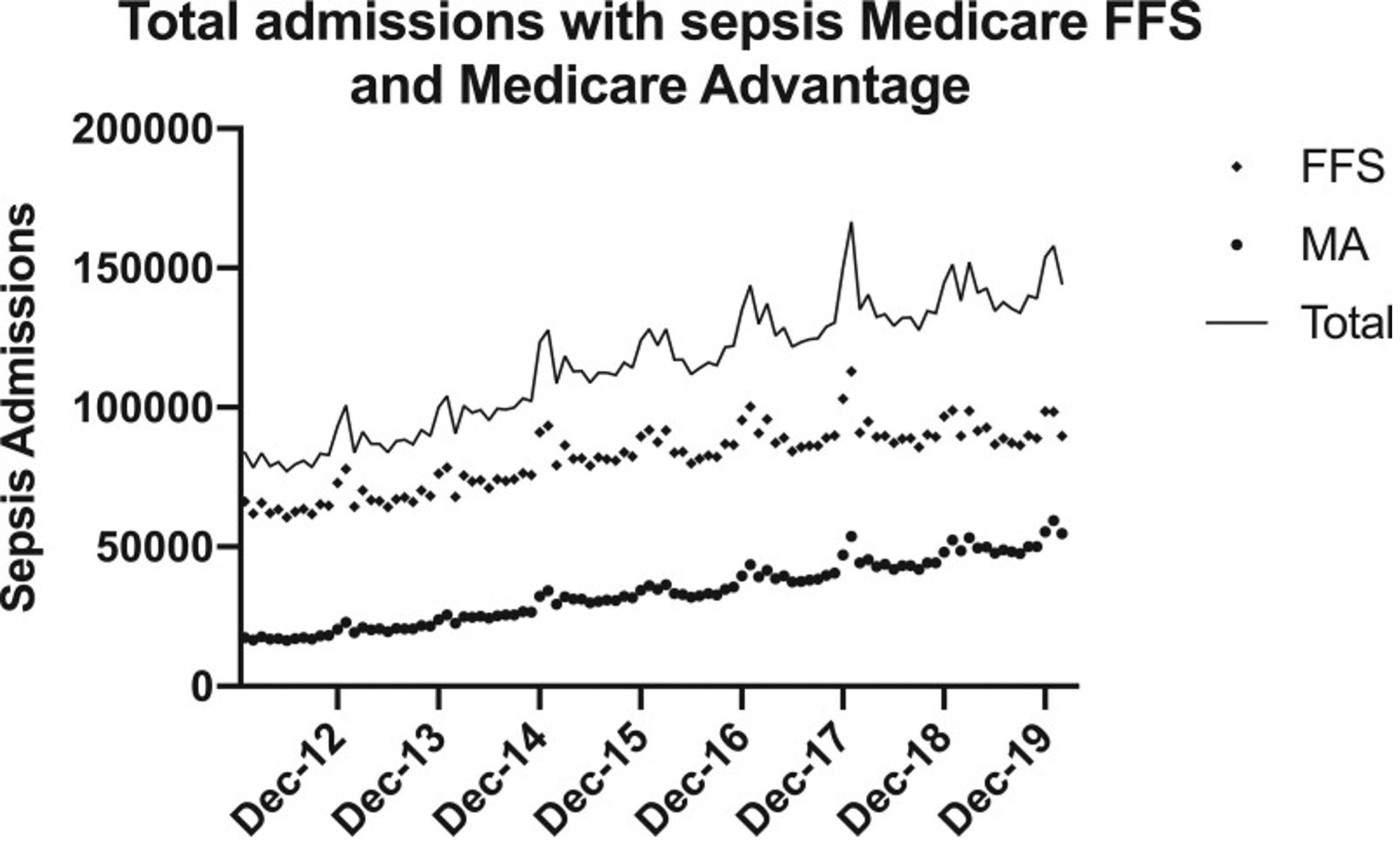
The HI-3 program collaborates across BARDA and other US Government Agencies to reduce the incidence, morbidity, and mortality of sepsis. Sepsis, which can arise from almost any infection, impacts around 1.7 million adults annually in the US, contributes to over 250,000 deaths, and leaves many survivors with long-term health challenges, making sepsis a critical public health threat.

The HI-3 program has made a strategic investment with the Sepsis Alliance to bring together subject matter experts from diverse stakeholder groups. The goal of this public-private partnership is to address unmet needs around infection management and sepsis prevention, detection, and treatment.
APPROACH
The HI-3 program is de-risking strategies for public health emergencies, but also piloting new solutions. We want to leverage insights gained from how care is sought and delivered in the real world to identify gaps in pandemic preparedness and address unmet clinical needs, expand to new care settings, and demonstrate ability to change clinical outcomes.
Our current areas of focus include:
- Support the infrastructure needed to clinically evaluate medical innovations, improve equity and access and deliver care in real-world health ecosystems
- Implement and assess the clinical utility of novel health products, technologies, care delivery models, and analytical approaches
- Drive impact through novel strategic stakeholder partnerships and illuminating the need for change from analytical insights
Program Goals
Increase Access to Care
Implement next generation health care and clinical study models
Power New Pandemic Preparedness Approaches
Strengthen ability to be agile to new threats
Address Unmet Clinical Needs
Identify gaps and foster strategic approaches to drive change
Demonstrate Real World Utility
Demonstrate the clinical value of new products, technologies, and delivery models in changing patient health journeys
HI-3
Past opportunities
The HI-3 program created the Pediatric COVID-19 Data Challenge to address gaps in our understanding of COVID progression in pediatric populations. Participants developed, trained, and validated computational models to predict pediatric patients' risk for negative clinical outcomes.